Ultrasound-guided Radial Arterial Line Placement
Insertion of a radial arterial catheter is a common procedure in critical care units. Radial artery catheters are commonly placed for continuous blood pressure monitoring, frequent arterial blood gas analysis, or frequent blood sampling for diagnostic testing.
Radial artery cannulation can be challenging and ultrasound guidance has emerged as a valuable adjunct for the placement of radial artery catheters. The advantages of ultrasound guidance include: real-time visualization of landmarks, improved pre-procedure planning, reduction in complications, less time spent at the bedside, and improved first-attempt success rates.
Which ultrasound scanner is best for radial arterial line placement?
The radial artery is identified using a linear or vascular probe SIFULTRAS-3.31. The probe is placed on the wrist where the pulse is palpated (or via anatomic landmarks if there is no palpable pulse) or along the forearm and wrist.
The traditional method for radial artery catheter placement is to locate the vessel via palpation of the pulse or anatomic landmarks. Unfortunately, anatomic landmarks may not locate the radial artery in up to 30% of patients.
In patients with severe hypotension, morbid obesity, and atherosclerosis, the radial pulse may be weak or absent, making locating the artery via palpation difficult.
Other difficulties commonly encountered during radial artery catheter placement include: the inability to thread the wire, hematoma formation, scarring from previous arterial catheters, atherosclerosis, and arterial spasm.
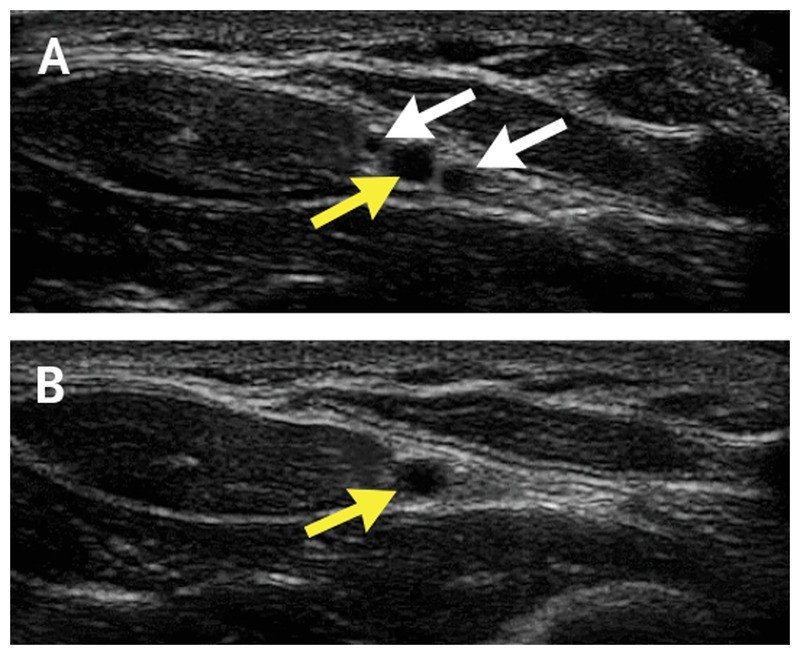
Different methods can be adopted for radial arterial mine placement. The first is the transverse method, where the probe is placed perpendicular to the artery. The second technique is the longitudinal method, where the probe is oriented parallel to the vessel. A third method is the static technique, where the vessel is identified via ultrasound, and a mark is made on the skin along the artery’s path with a sterile marker.
Ultrasound guidance has been shown to reduce complications and increase success rates for bedside clinicians, including respiratory therapists (RTs), during central venous catheter insertion.
Ultrasound guidance reduced the mean number of attempts required for successful catheter placement, reduced time to successful catheter placement, and reduced the number of hematomas.
Ultrasound guidance reduces the likelihood of hitting the nerve bundle and other structures near the artery due to real-time visualization of the needle as it approaches the artery and underlying structures. Ultrasound should minimize this difficulty and reduce the risk of vessel damage and morbidity because real-time guidance reduces the likelihood of hitting underlying structures, such as nerves, ligaments, and tendons.
Arterial lines are typically inserted by Physicians, Acute Care Nurse Practitioners (ACNP), ICU Physician Assistants (PAs), Anesthesiologist Assistants (CAAs), Nurse Anesthetists (CRNAs), and Respiratory Therapists.
References: Review of Ultrasound-Guided Radial Artery Catheter Placement, Ultrasound-Guided Insertion of a Radial Arterial Catheter.
Disclaimer: Although the information we provide is used by different doctors and medical staff to perform their procedures and clinical applications, the information contained in this article is for consideration only. SIFSOF is not responsible neither for the misuse of the device nor for the wrong or randomgeneralizability of the device in all clinical applications or procedures mentioned in our articles. Users must have the proper training and skills to perform the procedure with each vein finder device.
The products mentioned in this article are only for sale to medical staff (doctors, nurses, certified practitioners, etc.) or to private users assisted by or under the supervision of a medical professional.



