BPB : Brachial Plexus Block
BPB (Brachial plexus block) is a procedure performed by an Anesthesiologist in purpose to deliver regional anesthesia to the targeted area.
BPB are commonly achieved via an interscalene, supraclavicular, infraclavicular, or axillary approach.
Ultrasound machine with linear transducer (8–14 MHz), sterile sleeve, and gel (or other acoustic coupling agent; eg, saline) are needed for BPB.
The portable Ultrasound scanners guidance allows for visualization of the spread of the local anesthetic and additional injections around the brachial plexus if needed to ensure an adequate spread of local anesthetic, improving block success.
The Ultrasonography also offers the ability to visualize local anesthetic spread and to inject multiple aliquots also allows for a reduction in the volume of local anesthetic required to accomplish the block.
Interscalene Brachial Plexus Block:

With the patient in the proper position, the skin is disinfected and the transducer is positioned in the transverse plane to identify the carotid artery. Once the artery has been identified, the transducer is moved slightly laterally across the neck. The goal is to identify the anterior and middle scalene muscles and the elements of the brachial plexus that is located between them. It is recommended to use the color Doppler to identify vascular structures and avoid them.
The needle is then inserted in-plane toward the brachial plexus, typically in a lateral-to-medial direction, although a medial-to-lateral needle orientation can also be used if there is no room for the former. The needle should always be aimed in between the roots instead of directly at them in order to minimize the risk of accidental nerve injury.
Source: Ultrasound-Guided Interscalene Brachial Plexus Block
Supraclavicular Brachial Plexus Block:
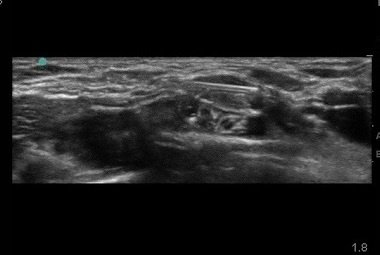
The ultrasound helps you locate and confirm the pulsatile, hypoechoic subclavian artery sitting on the hyperechoic line of the first rib or pleura. And to differ the carotid artery from the subclavian.
The subclavian vein is located medial to the artery. The brachial plexus lies lateral to the subclavian artery and superior to the first rib. The first rib appears hyperechoic with an underlying shadow. Identify the hyperechoic line of the pleura and compare it with the hyperechoic first rib.
After injecting anaesthetise the skin, insert the short bevel needle along the longitudinal axis of the ultrasound probe. By keeping the needle parallel to this axis the practitioner insures the visualization of the needle tip by all times. Insert the needle lateral to the probe aiming medially. Directing the needle toward the first rib rather than the pleura can reduce the risk of accidently puncturing the pleura.
Some practitioners therefore prefer a medial to lateral approach. This is theoretically safer as the needle movement is away from the lung. However, this approach requires expert manipulation of the needle, as the artery is in the path between the point of needle insertion and the corner pocket. In both techniques, the tip of the needle should be visualized at all times. Never advance the needle deep into the hyperechoic line of the rib/pleura.
Source: Ultrasound-Guided Supraclavicular Brachial Plexus Block.
Brachial plexus block is typically performed by an anesthesiologist.
[launchpad_feedback]
Disclaimer: Although the information we provide is used by different doctors and medical staff to perform their procedures and clinical applications, the information contained in this article is for consideration only. SIFSOF is not responsible neither for the misuse of the device nor for the wrong or random generalizability of the device in all clinical applications or procedures mentioned in our articles. Users must have the proper training and skills to perform the procedure with each ultrasound scanner device.
The products mentioned in this article are only for sale to medical staff (doctors, nurses, certified practitioners, etc.) or to private users assisted by or under the supervision of a medical professional.


